The topic of Artificial Intelligence (AI) is becoming widespread, gaining a lot of attention across many industries, and in some cases, causing some people to fear for the future of their jobs or careers. According to the Pew Research Center, there are industries that are most exposed to AI taking over, those are industries that require a high degree of education and analytical skills (Kochhar, 2023). Public Health is one of the industries where AI is gaining traction. Rather than replacing Public Health and Healthcare professionals, AI is partnering with these professionals and becoming an integrated tool in the profession.

Although Public Health and healthcare employ some of the most highly educated professionals such as physicians, advanced practice providers, nurses, pharmacists, social workers, and ancillary personnel; AI is a tool enhancing their efficiency and effectiveness. Consider a carpenter with power tools. Power tools did not replace carpenters, a well-made power tool that is effective made the carpenter more efficient. In an article published in the Wall Street Journal, the concept of innovation replacing human labor is not new. In fact, there are reasons to not fear the rise of robotics in the workforce. Author Greg Ip provides an example of the invention of the knitting machine back in 1500’s. He states, “’Robot apocalypse’ is a modern expression, but the underlying anxiety goes back centuries. In 1589 Queen Elizabeth I refused to grant the inventor of a mechanical knitting machine a patent for fear of putting manual knitters out of work” (Ip, 2017). As we learned, in many cases robotics changed the way work was done, not eliminating the trade or profession. In the case of knitters, the invention of the knitting machine allowed them to produce more at less cost. Could AI produce similar results in Public Health, producing more positive outcomes at less cost?
Public Health and AI
The use of artificial intelligence varies across many areas of public health such as building outbreak models and disease predictions, developing drugs, personalized regimen of medication, health risk models, and hospital resource management and operations. These technologies are already being used in hospitals and are getting an efficiency boost from AI. Hospitals have replaced paper charts with electronic health records (EHR) as well as the utilization or robotics in surgery such as Intuitive Surgical, Inc. popular da Vinci robot. As with all innovations, there are also ethical questions and dilemmas to consider.
Telemedicine and Machine Learning
As COVID-19 became a pandemic it rapidly changed how providers were delivering healthcare to patients. While communicating with patients remotely was a viable option prior to the pandemic, the pandemic made it a necessity as clinics and hospitals were filling up with patients suffering from COVID-19. People were encouraged not to see their healthcare providers unless it was an emergency, or they had symptoms of COVID-19. In a research survey by the American Medical Association, during the first year of the pandemic, 57% of respondence did not see their provider due to fear of COVID-19 exposure, 29% missed their preventative care visits, and 26% missed outpatient general medical appointments (Henry, 2021).
When Telemedicine was first being rolled out, the basic device was a screen with a camera and microphone; similar experience as a regular tele video meeting or conference call. More sophisticated devices allowed for a language interpreter to join the call and even provide options for additional providers to join and consult with the patient, dictate the encounter, and upload the consult into an EHR. With the induction of AI, telemedicine is becoming more sophisticated and assisting providers with triage, diagnosis, and treatment.
With the assistance of machine learning (ML), patients can communicate with chatbots identifying patterns assisting in triaging patients to the appropriate medical provider. Clinics in Singapore utilized a platform known as Bot MD Care that used popular platforms such as WhatsApp and Messenger. The Bot MD platform was paramount during the pandemic by monitoring vitals and triaging over 4000 patients and would send out reminders and enable follow-up via video consultation using the popular chat platforms (World Health Organization, 2022). On the other end, the clinician or medical provide will receive the patient’s data and information to assist in diagnosis (Tiribelli, et al., 2023).
Monitoring and Reporting
Many people today carry some sort of smart device such as a smart phone or a fitness monitoring device. When AI and ML are introduced to these devices, they can monitor the patient looking for specific patterns and report any deviations that could be caused by a condition to the patient’s health care provider. Trackers and smart devices today can monitor heart rate, oxygen saturation, blood pressure, and even glucose levels. Individuals can track and monitor their own vitals. More advanced system can be placed into nursing homes and look for other signs such as early onset of Parkinsons or notify if someone may become a fall risk (Tiribelli, et al., 2023). These tracking devices can only monitor and look for patterns that could potentially be a cause of early onset of a disease. It is still up to the provider to do further studies to properly diagnose patients.
Facial Recognition
Beyond security identification and surveillance, facial recognition integrated in telemedicine can assist the provider in identifying potential clues to a patient’s condition or change in lifestyle. Similar to smart devices monitoring patterns, facial recognition and ML will monitor a patient’s facial shape and structure and then track any changes to determine if a patient is potentially gaining or losing weight or if there is a change in skin color that could be a sign of a skin condition or lack of antioxidants in a person’s diet. In a research study published in Frontiers in Psychology, it identifies many of the applications as to how facial recognition can identify risk factors for cardiovascular illness; however, considering the unique physiology of patients based on race and gender, there have been mixed results linking facial appearance to physiological health (Stephen, Hiew, Coetzee, Tiddeman, & Perrett, 2017).
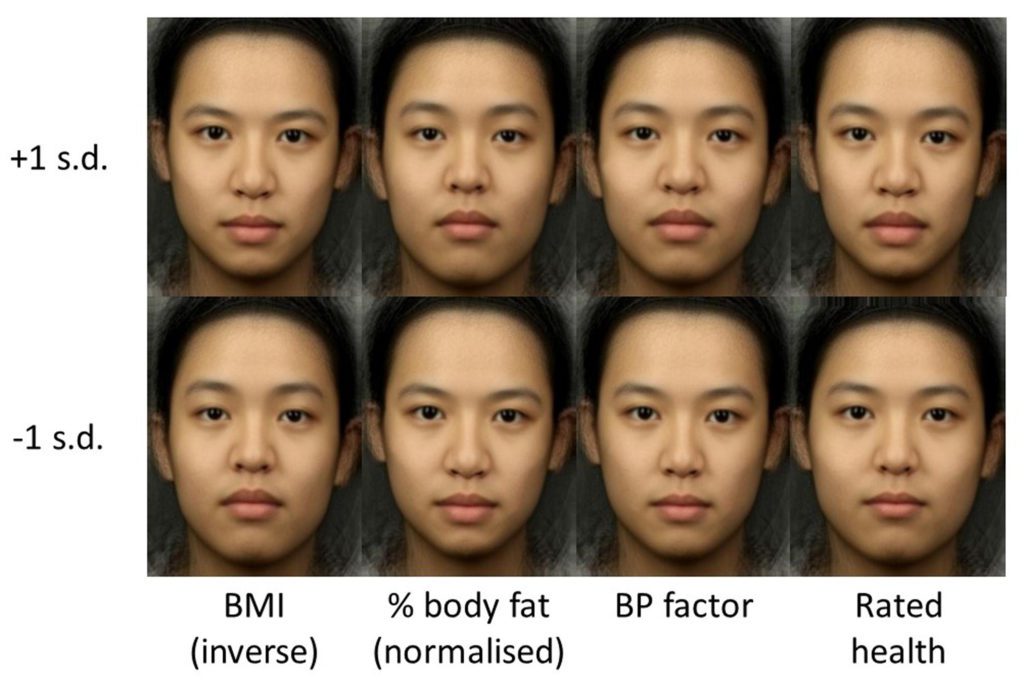
normalized percentage fat, blood pressure factor, and health rating.
Source: Stephen, I. D., Hiew, V., Coetzee, V., Tiddeman, B. P., & Perrett, D. I. (2017). Facial Shape Analysis Identifies Valid Cues to Aspects of Physiological Health in Caucasian, Asian, and African Populations. Frontiers in psychology, 8, 1883. https://doi.org/10.3389/fpsyg.2017.01883
Limitation of Artificial Intelligence
While AI and ML play an important role and provide a new tool for healthcare providers, there are limitations and possibilities for bias. Among some of the limitations are women’s natural tendencies to have a higher BMI than men possibly to naturally facilitate childbirth (Stephen, Hiew, Coetzee, Tiddeman, & Perrett, 2017). Another limitation to potential bias would be the disparity of patient encounters of a certain race or ethnicity. If the device does not have an adequate number of patients of a particular race to study, it may cause some inaccuracies in its diagnosis. Skin conditions could be missed or misinterpreted by people of different skin color. Within the past few years, telemedicine has evolved from a mere device for telecommunicating, to smart devices that can monitor and alert medical providers of potential health care risks and diagnosis. As sophisticated as AI and ML are, in telehealth, it cannot replace the medical professional in diagnosis and treatment. AI and ML are just another set of tools to assist the providers to better effectively diagnosis patients of the potential onset of any health risks or diseases putting these patients another step closer to treatment.
References
- Henry, T. A. (2021, February 15). Why 41% of patients have skipped care during COVID-19 pandemic. Retrieved from https://www.ama-assn.org/: https://www.ama-assn.org/delivering-care/public-health/why-41-patients-have-skipped-care-during-covid-19-pandemic
- Ip, G. (2017, September 5). Workers: Fear Not the Robot Apocalypse. Wall Street Journal.
- Kochhar, R. (2023, July 26). Which U.S. Workers Are More Exposed to AI on Their Jobs? Retrieved from Pew Research Center: https://www.pewresearch.org/social-trends/2023/07/26/which-u-s-workers-are-more-exposed-to-ai-on-their-jobs/
- Stephen, I. D., Hiew, V., Coetzee, V., Tiddeman, B. P., & Perrett, D. I. (2017). Facial Shape Analysis Identifies Valid Cues to Aspects of Physiological Health in Caucasian, Asian, and African Populations. Frontiers in Psychology, 1-10.
- Tiribelli, S., Monnot, A., Shah, S. F., Arora, A., Toong, P. J., & Kong, S. (2023). Ethics Principles for Artificial Intelligence–Based Telemedicine for Public Health. American Journal of Public Health, 577-584.
- World Health Organization. (2022, April 25). WHO Western Pacific Innovation Challenge Bot MD. Retrieved from www.who.int: https://www.who.int/westernpacific/initiatives/innovation-for-health-impact/innovation-challenge/bot-md



[…] remote or telemedicine assisting providers with identifying diseases, diagnosis, and treatments (Introduction to AI and Telemedicine). One of the most groundbreaking applications of AI in healthcare is AI-assisted surgery. This […]