Consider a person not having any sun exposure for two years completely bundled up and remain indoors with no sunlight or UV rays. Two years later that person goes outside into the summer heat with no sun protection of any kind and a UV index of 8+ for one hour. Chances are that person will suffer significant sun burns due to a lack of pigmentation caused by a deficiency of natural UV exposure and melanin (Solano, 2020). Although it is not advisable to be outside without protection when the UV index is high, pigmentation does help in the development of sun tolerance. Just like moderate exposure to the sun and UV rays are beneficial developing sun tolerance and a good source of vitamin D, moderate exposure to our environment is also beneficial in the development of our immune system. As we are coming out of the COVID-19 pandemic and people are returning to what is considered normal living, many children are contracting and becoming ill to Respiratory Syncytial Virus or RSV. While the world was on lockdown shielding itself from the environment and social gatherings, this apparently caused an immunity deficiency. This deficiency is blamed for the severe cases of illnesses such as RSV developing with more intensity that it has pre COVID-19 pandemic.
According to the Centers for Disease Control and Prevention (CDC), there has been an increase in cases and emergency department visits due to RSV (Centers for Disease Control and Prevention, 2022). RSV is not a new disease. Its first recorded case was in 1956 and is most common in infants and children; a major contributing factor in childhood pneumonia (Chanock, et al., 1962). In a recent study out of the U.K. from the London School of Hygiene & Tropical Medicine, the contributing factor to this increase of cases could be due to the COVID-19 pandemic restriction imposed upon children worldwide early 2020 (Koltai, 2022). When the SARS-CoV-2 was identified as a pandemic early March, there was no vaccine or effective treatment for those who contracted the disease. In response to the slow the spread of the virus, non-pharmaceutical interventions (NPI) were implemented. Governments forced the shutdowns of businesses and schools, advised social distancing, and mandated face mask wearing in public indoor and outdoor settings. According to the study, the NPI caused a disruption in the normal development of the immune responses to seasonal viruses such as the flu and RSV (Koltai, 2022). As the NPI began to relax, there began an increase in cases of RSV among children as lack of repeated exposure caused an immune deficiency.
In the U.K. study, researchers charted the cases the two years prior to the pandemic and noticed RSV season patterns in the graph (figure 1 and 2). Cases would typically begin to rise around October, peeking in December, and begin its decline throughout the remining weeks of winter. In the beginning of 2020, RSV declined as it typically does, and cases flatten right before Spring; this is its normal pattern. In March 2020 began the COVID-19 pandemic and governments began shutting down schools, businesses, and mandated NPI protocols such as wearing a mask. Even as businesses started to reopen around summer of 2020 several measures were put into place such as acrylic or plastic shields in retail spaces and continued mask wearing indoors. Schools remained online preventing children from gathering. In the attempt to flatten the COVID-19 curve, these mandates caused a flattened the seasonal RSV curve and very few cases and hospitalization of RSV was reported during the fall of 2020 through winter. As COVID-19 vaccines became available people began gathering more and NPI mandates were being lifted, RSV infections began to rise. According to the graph, the RSV infections and hospitalization started in the summer of 2021, earlier than its typical seasonal trend. In 2022, with nearly all NPI for COVID-19 removed, the CDC is reporting huge increase in RSV cases and hospitalizations.
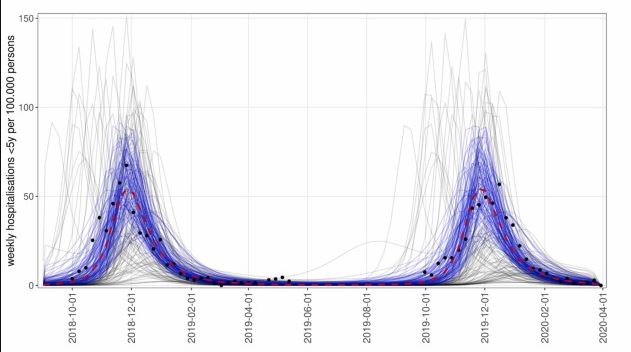
Fig 1. Simulated hospitalisations for children under 5 years before the COVID-19 pandemic. Source: Koltai, M. K.-S. (2022). Determinants of RSV epidemiology following suppression through pandemic contact restrictions. Epidemics, 40.
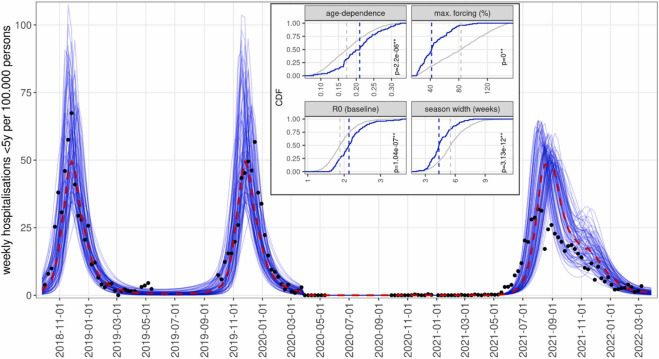
Fig 2. Simulations of RSV resurgence from June 2021, assuming gradual recovery of contact levels from March 2021, showing the 10% of simulations with the lowest error with respect to SARI-Watch hospitalization rates. Source: Koltai, M. K.-S. (2022). Determinants of RSV epidemiology following suppression through pandemic contact restrictions. Epidemics, 40.
Discussion
While during the COVID-19 pandemic there were discussions between the balance of public health and safety and personal freedom and rights, the unintended consequences on natural immunity was overlooked or ignored. RSV is not a new virus and children frequently do get exposed to the virus. The normal gathering of children most likely kept their immune system active to fight off any major symptoms caused by RSV. Forcing children to not congregate and wear personal protective equipment (PPE) like facemasks, weakened the immune system preventing it from effectively fighting off the RSV. This natural congregation became the natural booster for the RSV preventing or mitigating serious illnesses in children.
While PPE and physical distancing can help reduce the spread of a diseases, public health officials must be cognizant of prolonged use and how it can disrupt the natural immune system. In the case of the RSV, precautions to slow the spread of COVID-19 caused an immune deficiency for RSV.
References
Centers for Disease Control and Prevention. (2022, October 28). Respiratory Syncytial Virus Infection (RSV). Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/rsv/index.html
Chanock, R. M., Parrott, R. H., Vargosko, A. J., Kapikian, A. Z., Knight, V., & Johnson, K. M. (1962). Respiratory Synsytal Virus. American Journal of Public Health, 918-925.
Koltai, M. K.-S. (2022). Determinants of RSV epidemiology following suppression through pandemic contact restrictions. Epidemics, 40.
Solano, F. (2020). Photoprotection and Skin Pigmentation: Melanin-Related Molecules and Some Other New Agents Obtained from Natural Sources. Molecules, 1537.